Endocrine glands
- Endocrine glands are glands of the endocrine system that secrete their products, hormones, directly into the blood rather than through a duct.
- The major glands of the endocrine system include the pineal gland, pituitary gland, pancreas, ovaries, testes, thyroid gland, parathyroid gland, hypothalamus and adrenal glands.
Hormones from anterior pituitary gland
Hormones from anterior pituitary gland are as follows:
- Growth hormones: Promote growth of whole body, particularly of the skeleton.
- Thyroid stimulating hormone: Stimulates thyroid to secrete thyroxine.
- Adrenocorticotropic hormone: Stimulate adrenal cortex.
- Gonadotrophic hormone: Regulates the activity of gonads (testes and ovaries).
Adrenal gland- Detailed structure

The adrenal gland is a small triangular-shaped gland located on top of each kidney. The gland is made of two types of tissues; The adrenal cortex (outer tissue) and the adrenal medulla (central tissue).
Adrenal Cortex is divided into three layers
Adrenal Cortex is divided into three layers
- Zona reticularis (innermost layer)
- Zona fasciculata (middle layer)
- Zona glomerulosa (outer layer)
- The adrenal cortex region is controlled by the pituitary gland
- It produces the corticosteroid hormones also called the corticoids and the androgens (male sex hormones)
- It is an integral part of the autonomous nervous system
- The medulla is made of chromaffin cells that synthesize and secrete the catecholamines.
- The chromaffin cells have the ability to convert the amino acid tyrosine to catecholamines.
Adrenal gland- Origin and location
The Adrenal glands present on the kidneys, secrete various hormones which control several critical processes in the body. It has 2 parts the adrenal cortex and the adrenal medulla
Origin
Origin
- The Adrenal cortex develops from intermediate mesoderm while the Adrenal medulla develops from the ectoderm of the embryo.
- One pair of adrenal glands is present in the body. One adrenal gland is located at the anterior part of each kidney.
Adrenal cortex
The adrenal gland is a small triangular-shaped gland located on top of each kidney. The gland is made of two types of tissues; The adrenal cortex (outer tissue) and the adrenal medulla (central tissue).
Adrenal Cortex is divided into three layers
Adrenal Cortex is divided into three layers
- Zona reticularis (innermost layer)
- Zona fasciculata (middle layer)
- Zona glomerulosa (outer layer)
- The adrenal cortex region is controlled by the pituitary gland
- It produces the corticosteroid hormones also called the corticoids and the androgens (male sex hormones)
Hormones secreted by adrenal cortex
Hormones secreted by adrenal cortex are as follows:
- Mineralocorticosteroids (aldosterone): Regulates plasma, sodium and potassium concentrations
- Glucocorticosteroids (cortisol, corticosterone): Regulates carbohydrate, protein and lipid mechanism.
- Sex corticoids (adrenal androgens): Stimulates development of external sex characters in males.
Pineal gland- Origin, location and structure

Pineal gland is also called as pineal body or epiphysis or the third eye.
Origin
Origin
- Develops from the Ectoderm of the embryo
- It is located behind the third cerebral ventricle on the dorsal side of the fore brain
- It has a pine-cone like structure and consists of pineal cells and supporting glial cells.
- It lower vertebrates it has an eye-like structure and acts as a light receptor (hence the name third eye)
Hormones of the pineal gland
The Pineal gland produces only one hormone called the melatonin. The functions of melatonin are as follows
- Both melatonin and its precursor called serotonin are synthesized in the pineal gland
- Tryptamine (an alkaloid substance) is the precursor for both melatonin and serotonin.
- Melatonin plays an important role in the diurnal rhythm (e.g. sleep-wake cycle) of the body.
- Melatonin causes a sense of drowsiness (sleepiness) in the brain at night time, which affects the modulation of sleep patterns.
- Melatonin also influences metabolism, pigmentation, menstrual cycle and immunity.
Thymus gland- Origin, location and structure

Thymus gland is a gland that is closely associated with the immune system than the endocrine system. It grows in size until puberty and then starts to shrink as we age. It secretes hormones only till pre-pubescence.
Origin
Origin
- Develops from the endoderm of the embryo
- It is located in the upper chest region beneath the breastbone in front of the heart
- It is a soft, roughly triangular, bilobed mass of lymphoid tissue.
- The shape resembles that of a thyme leaf.
- The external surface of the thymus is covered by a connective tissue called the capsule.
- Each lobe of the thymus is divided into several lobules. The outer zone of the lobe is called the cortex and the inner zone is called the medulla.
- The thymus is mainly made of two types of cells; the lymphocytes and the reticular cells
Hormones of the Thymus gland
The thymus actively secretes the hormones called thymosins (only till pre-pubescence) Thymosins are peptide hormones which play an important role in
- The stimulation, development and differntiation of T-lymphocytes.
- The development of cell-mediated immunity (T-lymphocytes mediated immunity)
- The production of antibodies (Humoral immunity).
Function of hormones secreted by pancreas
The three main hormones produced by the endocrine pancreas and their functions are
Glucagon
Glucagon
- It is a polypeptide hormone.
- It is secreted by the pancreas when the glucose level in the blood drops.
- It increases the blood glucose levels by initiating glycogenolysis (glycogen degradation) and stimulating gluconeogenesis (synthesis of glucose from non-carbohydrate molecules) in the liver cells.
- Since it increases the blood glucose levels it is a hyperglycemic (hyper-more, glycemic-sugar levels) hormone
- It also initiates lipolysis (degradation of lipid) in the adipose tissue.
- It is also a polypeptide hormone
- It has antagonistic (opposite) effects of the hormone glucagon.
- It is released when the glucose level in the blood raises.
- It lowers blood sugar levels in different ways; increasing the uptake of glucose by all the cells in the body, initiating glycogenesis (glycogen synthesis) in the liver and muscle.
- It initiates lipogenesis (synthesis of lipids/fat) and storage of fat in adipose tissue and inhibits gluconeogenesis
- It is a hypoglycemic (hypo=less) hormone as it reduces the sugar levels in the blood
- Also known as growth hormone-inhibiting hormone (GHIH)
- It acts locally on the Islets of Langerhans and inhibit the secretion of both insulin and glucagon
- It also reduces gastric secretions and inhibits the release of gastrointestinal hormones
- It is a polypeptide secreted by the cells of the pancreas.
- Protein is strong stimulus for its production
- It affects gastric and biliary secretion and motility of the GI tract
Extrenal structure of pancreas
- The pancreas comprises of head, neck, body and tail.
- The main pancreatic duct is formed from smaller ducts within the pancreas, which opens into hepatopancreatic ampulla.
- An accessory duct is also present in pancreas which opens directly into the duodenum.
Hormones of the Pancreas
The hormones produced by the endocrine pancreas and their functions are
Glucagon
Glucagon
- It is a polypeptide hormone.
- It is secreted by the pancreas when the glucose level in the blood drops.
- It increases the blood glucose levels by initiating glycogenolysis (glycogen degradation) and stimulating gluconeogenesis (synthesis of glucose from non-carbohydrate molecules) in the liver cells.
- Since it increases the blood glucose levels it is a hyperglycemic (hyper-more, glycemic-sugar levels) hormone
- It also initiates lipolysis (degradation of lipid) in the adipose tissue.
- It is also a polypeptide hormone
- It has antagonistic (opposite) effects of the hormone glucagon.
- It is released when the glucose level in the blood raises.
- It lowers blood sugar levels in different ways; increasing the uptake of glucose by all the cells in the body, initiating glycogenesis (glycogen synthesis) in the liver and muscle.
- It initiates lipogenesis (synthesis of lipids/fat) and storage of fat in adipose tissue and inhibits gluconeogenesis
- It is a hypoglycemic (hypo=less) hormone as it reduces the sugar levels in the
- Also known as growth hormone-inhibiting hormone (GHIH)
- It acts locally on the Islets of Langerhans and inhibit the secretion of both insulin and glucagon
- It also reduces gastric secretions and inhibits the release of gastrointestinal hormones
- It is a polypeptide secreted by the $$\gamma$$ cells of the pancreas.
- Protein is strong stimulus for its production
- It affects gastric and biliary secretion and motility of the GI tract
Disorders of pancreas
Two major disorders associated with pancreas
Hyperglycemia
Hyperglycemia
- It is due to deficiency of insulin.
- Its symptoms are high blood glucose level, breakdown of muscle tissue and tiredness.
- It is due to excess of insulin.
- Its symptoms are low blood glucose level, hunger, sweating, irritability and double vision.
Thyroid gland- Origin, location and structure

The thyroid gland is an endocrine gland in the neck.
Origin
Origin
- Develops from the endoderm of the embryo
- It is located at the base of the neck just below Adam's apple. Anterior to the thyroid cartilage of the larynx in the neck.
- It is butterfly shaped, bilobed organ.
- The two lobes are interconnected with a tissue called isthmus.
- It contains 2 types of tissues; Follicles and stromal tissues
- Follicles are made of follicular cells which synthesize the thyroid hormones
- The stromal tissue forms the connective tissue that supports the follicular cells.
Disorders of Thyroid gland
The two most common disorders associated with the thyroid gland are the hyperthyroidism and the hyporthyroidism.
Hyperthyroidism
Hyperthyroidism
- It is condition in which is the thyroid is overactive i.e. there is overproduction (higher than normal) of thyroid hormones.
- It is condition in which is the thyroid is underactive i.e. there is underproduction (lower than normal) of thyroid hormones.
Function of hormones secreted by thyroid gland
The follicular cells of the thyroid gland synthesize two thyroid hormones; Tetraiodothyronine ( $$T_4$$-Thyroxine) and triiodothyronine ( $$T_3$$) and the C-cells of thyroid gland produces Thyrocalcitonin. The function of these hormones are as follows
- Thyroxine is the main hormone (80% in thyroxine form) secreted into the bloodstream by the thyroid gland.
- It is the inactive form and most of it is converted to an active form called as triiodothyronine $$T_3$$ by organs such as the liver and kidneys.
- Both $$T_4$$ and $$T_3$$ are synthesized from tyrosine and iodine.
- The thyroid hormones control the metabolism of carbohydrates, protein and fats. They play an important role in regulating the Basal Metabolic Rate (BMR)
- They are also important for maintenance of water and electrolyte balance.
- Thyroid hormones also regulate the RBC production.
- The thyrocalcitonin maintains the blood calcium levels and promotes the bone formation.
Disorders of thyroid gland- Hypothyroidism
Hypothyroidism, also called underactive thyroid disease, is a common disorder in which the thyroid gland does not make enough thyroid hormone.
Causes
Causes
- Simple goitre or endemic colloid goitre
- Hashimoto disease
- Surgical removal of thyroid gland
- Use of certain drugs (Lithium, some cold and sinus medication)
- Exposure to radiation (irradiation)
- Genetic disorder (genetic defect of the thyroid gland)
- Extreme muscular sluggishness
- Decreased heart rate, cardiac output and blood volume
- Scaly skin
- Froglike husky voice
- Gain in body weight
- Myxedema (bagginess under the eyes and swelling of the face)
- Cretinism (failure of body growth and mental retardation)
Disorders of thyroid gland- Hypothyroidism- Hashimoto disease
Hashimoto disease is another common reason for hypothyroidism.
- It is an autoimmune disorder
- Antibodies are generated against thyroid gland
- The antibodies attack the thyroid tissue causing thyroiditis (inflammation of thyroid)
- This leads to progressive deterioration (decay) and finally fibrosis of the gland.
- The gland stops to secrete the thyroid hormones leading to hypothyroidism
Disorders of thyroid gland- Hypothyroidism- Myxedema
Almost total lack of thyroid function leads to a condition called myxedema.
In addition to the characteristics of hypothyroidism, they have certain symptoms like
Charatcteristic features
In addition to the characteristics of hypothyroidism, they have certain symptoms like
Charatcteristic features
- Bagginess under the eyes and swelling of the face
- Swelling and thickening of skin anywhere on your body, especially in lower legs (due to Increased hyaluronic acid and chondroitin sulphate deposits)
Disorders of thyroid gland- Hypothyroidism- Cretinism
Extreme hypothyroidism during fetal life, infancy or childhood can lead to cretinism.
Types
Types
- Congenital cretinism- cretinism due to the absence of thyroid gland (from birth) or due to failure of thyroid gland to produce thyroid hormones (because of a genetic defect in the thyroid gland)
- Endemic cretinism- cretinism due to iodine defeciency.
- Physically and mentally challenged.
- Obesity
- Short and stock appearance
- Large tongue
- Impaired skeletal growth
- Hypothyroidism
Disorders of thyroid gland- Hypothyroidism- Simple Goitre
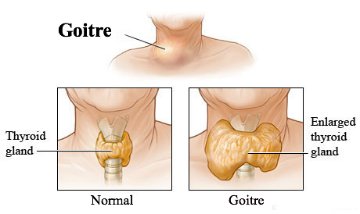
The term goitre means a greatly enlarged thyroid gland. If it occurs due to iodine deficiency in food, It is called simple or endemic colloid goitre
Thyroid hormones (both $$T_3$$ and $$T_4$$) are made from 2 components; tyrosine and iodine
About 50 milligrams of iodine/year is required for the formation of sufficient amount of thyroid hormone.
Insufficient iodine in the diet leads to endemic goitres.
Steps involved in thyroid hormone release
Thyroid hormones (both $$T_3$$ and $$T_4$$) are made from 2 components; tyrosine and iodine
About 50 milligrams of iodine/year is required for the formation of sufficient amount of thyroid hormone.
Insufficient iodine in the diet leads to endemic goitres.
Steps involved in thyroid hormone release
- For the production of thyroid hormones by the thyroid gland, the TSH (Thyrotropin Releasing hormone from the anterior pituitary gland) should bind to TSH receptors of the thyroid gland
- Binding of TSH to TSH receptors stimulates the synthesis of a protein called thyroglobulin which is responsible for the synthesis of both $$T_3$$ and $$T_4$$
- Once they are synthesized by the thyroglobulin protein they are released into the blood.
- Soon after their release, they inhibit the production of TSH (since the body already made sufficient amounts of thyroid hormones) thereby regulating the thyroid hormone production.
- Lack of iodine prevents the production of both $$T_3$$ and $$T_4$$.
- As a result, no hormone is available to inhibit production of TSH by the anterior pituitary.
- So, the pituitary continues to secrete excessively large quantities of TSH.
- The TSH then stimulates the thyroid cells to secrete tremendous amounts of thyroglobulin
- Thyroglobulin cannot synthesize and release $$T_3$$ and $$T_4$$ because of lack of Iodine.
- No $$T_3$$ and $$T_4$$ release, so, no inhibition of TSH production.
- Continuous TSH production leads to continuous stimulation of the thyroid gland resulting in the production of more and more thyroglobulin.
- The gland grows larger and larger (10 to 20 times normal size) because of formation of excess thyroglobulin.
- All the symptoms associated with hypothyroidism can be seen in this simple or endemic colloid goitre
Disorders of thyroid gland- Hyperthyroidism- Graves' disease
Graves' disease is the most common reason for hyperthyroidism.
- It is an autoimmune disorder.
- Antibodies are generated against Thyrotropin stimulating receptor (TSH/thyrotropin receptor) in the thyroid gland
- These antibodies called the thyroid-stimulating immunoglobulins (TSIs) bind to the TSH receptor
- TSIs binding to the TSH receptor (the receptors that were supposed to bind TSH) leads to the continuous production of thyroid hormone by the thyroid gland.
- Excess production of thyroid hormone leads to hyperthyroidism.
Hyperthyroidism
Hyperthyroidism is a disorder in which your thyroid gland makes and releases more thyroid hormone than the body needs.
Causes
Causes
- Graves' disease
- Thyroid adenoma (tumor in thyroid gland)
- Toxic goiter [different from endemic colloid goiter caused by dietary Iodide deficiency (hypothyroidism)]
- Increased sweating
- mild to extreme weight loss
- Muscle weakness
- Exophthalmos - protrusion of eyeballs (due to swelling of the ocular/eye muscles )
- High state of excitability (quick reactions)
- intolerance to heat
- Tremors of the hands
- Diarrhea
- Nervous disorders
- Extreme fatigue
- Inability to sleep
Movement in plant which are growth independent
- When we touch the leaves of a sensitive plants like 'touch me not' the plant folds its leaves and droops.
- This movement of the leaves and stem are totally because of the external stimulus touch.
- This type of movement is growth independent movements.
Hypothyroidism
A condition in which the thyroid gland doesn't produce enough thyroid hormone (thyroxine).
Causes
Causes
- They are many disorders that cause hypothyroidism; autoimmune disorders (e.g. Hashimoto's disease - autoantibodies against thyroid), iodine deficiency, pituitary disease, certain medications etc.
- Fatigue
- Depression
- Memory loss
- Dry and rough skin
- Joint and muscle pain
- Weight gain and
- inability to tolerate pain
Hormones of the Testis
The testis produces various male hormones collectively called as the androgens.
- The androgens include; testosterone, dihydrotestosterone and androstenedione.
- Testosterone is considered to be the primary hormone as it is produced abundantly when compared to others.
- However, dihydrotestosterone is the more active form. The testosterone is ultimately converted to the active form in the target tissues.
- Androgens regulate the development, maturation and function of the male sex organs (e.g. epididymis, seminal vesicles etc.,)
- They play an important role in spermatogenesis and male sexual behaviour
- They also promote protein and carbohydrate synthesis.
Testis- Origin, Location and Structure

Testis are the male gonads which are the most important organs of the male reproductive system.
Origin
Origin
- Develops from three different layers; The mesothelium (coelomic epithelium), the mesenchyme (intermediate mesoderm) and the primordial germ cells.
- These are present in a skin pouch called the scrotum located between the upper thighs
- They are oval-shaped organs
- They are made of approximately 900 seminiferous tubules and connective tissue called the stromal or interstitial tissue made of Leydig cells (present adjacent to the seminiferous tubules)
- The seminiferous tubules consists of seratoli cells along with spermatocytes, spermataozoa and the spermatids.
- The Leydig cells secrete the androgens (male sex hormones) and the seratoli cells are important for the formation of testis and the spermatogenesis.
Ovaries- Origin, location and structure
The ovaries are the female gonads that are essential organs of the female reproductive system
Origin
Origin
- Develops from three different layers; The mesothelium (coelomic epithelium), the mesenchyme (intermediate mesoderm) and the primordial germ cells.
- The ovaries lie in a shallow depression called the ovarian fossae, one on each side of the uterus.
- They have an ovoid shape.
- The ovary has 3 layers; the surface layer, the cortex and the medulla.
- The surface layer is also called the germinal epithelium (made of simple cuboidal epithelium)
- The cortex is made of follicles (surrounded by follicular cells) and connective tissue called the stroma.
- Estrogen is made by the follicles and hormone-producing tissue in the stroma.
- Medulla consists of supporting stroma and contains rich neurovascular network.
Hormones of the Ovary
The ovaries secrete two types of female sex hormones called the estrogens and the progestins.
Estrogens
Estrogens
- In Non-pregnant females, they are predominantly secreted by the ovaries. However, during pregnancy, the placenta secretes a lot of estrogens.
- The three types of estrogens are; $$\beta$$-estradiol, estrone and estriol.
- The most active and the principal estrogen produced by the ovaries is the $$\beta$$-estradiol.
- They play an important role in the growth and development of ovarian follicles and breast
- They are responsible for the development of secondary sexual characteristics (e.g. high pitch voice)
- They inhibit osteoclastic activity and stimulate bone growth. Osteoporosis in menopausal women is because of reduced estrogen levels.
- They also influence the texture of the skin and female sexual behaviour
- The progestins are secreted by the corpus luteum, a structure that is formed from the ruptured follicle (after ovulation/ later half of ovarian cycle).
- Most important progestin is the progesterone. Small amounts of 17-$$\alpha$$-hydroxyprogesterone is also secreted along with progesterone.
- Placenta also secretes large amounts of progesterone during pregnancy.
- The progestins mainly have 2 functions; prepare the uterus for pregnancy and prepare breasts for lactation.
- Progesterone acts on mammary glands and stimulates the formation of milk storing sacs called alveoli and milk secretion.
Inhibin/actin
Inhibin and Activin are two protein (cytokine) molecules with hormonal activity.
Inhibin
Inhibin
- Produced by both males and females.
- In males, it is secreted by the Sertoli cells and in females, it produced by multiple organs like the gonads, pituitary gland, placenta, corpus luteum etc.
- It inhibits FSH (Follicle Stimulating Hormone) production in both males and females.
- In males, it regulates the spermatogenesis process and in females, it regulates the menstrual cycle.
- It is also produced in both males and females. In males, it is produced in the testes, epididymis, prostate etc. and in females, it is produced by gonads and placenta etc.
- It stimulates the production of FSH and play an important role in the testicular and ovarian development
Inhibin and activin
Inhibin and Activin are two protein (cytokine) molecules with hormonal activity.
Inhibin
Inhibin
- Produced by both males and females.
- In males, it is secreted by the Sertoli cells and in females, it produced by multiple organs like the gonads, pituitary gland, placenta, corpus luteum etc.
- It inhibits FSH (Follicle Stimulating Hormone) production in both males and females.
- In males, it regulates the spermatogenesis process and in females, it regulates the menstrual cycle.
- It is also produced in both males and females. In males, it is produced in the testes, epididymis, prostate etc. and in females, it is produced by gonads and placenta etc.
- It stimulates the production of FSH and play an important role in the testicular and ovarian development
Control by anti natriuretic factor (ANF)
- A peptide called Atrial Natriuretic Factor (ANF), opposes the regulation by RAAS.
- The walls of the atria of the heart release ANF in response to an increase in blood volume and pressure.
- ANF inhibits the release of renin from the JGA, and thereby inhibits NaCl reabsorption by the collecting duct and reduces aldosterone release from adrenal gland.
- Thus ADH, RAAS and ANF provide an elaborate system of checks and balance that regulate the kidney functioning, to control body osmolarity, salt concentrations, blood pressure and blood volume.
Mode of steroid hormone action through intracellular receptor
- Hormones influence the growth and develop of organisms.
- For example, hormones determine whether individuals become male or female. Many hormones are steroids. Steroids are a class of lipids. All steroids share a carbon skeleton composed of four fused rings.
- Hormones are compounds used for long distance signaling in both plants and animals.
- In animals, specialized cells produce hormones and release them into the circulatory system.
- Hormones travel to target cells in other parts of the body and cause a variety of changes in the target areas.
- Changes caused by hormones include changes in gene expression in target cells as well as steroid hormones are soluble in lipids and can easily pass through cellular and nuclear membranes. In contrast, many other hormones are water soluble.
- Steroid hormones typically act by affecting gene expression while water-soluble hormones usually act by causing changes in biological processes in the cytoplasm of cells.
Formation of hormone receptor complex
- Binding of insulin to the outer subunits of the receptor causes a conformational change in the membrane spanning subunits, which is also an enzyme, a tyrosine kinase.
- The activated subunits add phosphate groups of specific tyrosine residues located in cytoplasmic domain of the receptor, as well as a variety of insulin receptor substrates.
Formation of secondary messengers
- As a result of -subunit activity, a transducer G protein activates enzyme phosphodiesterase.
- This enzyme makes phosphatidylinositol 4,5-biphosphate (PIP2) into a pair of mediators inositoltriphosphate (IP3) and diacylglycerol (DG).
- In turn, IP3, which is water-soluble, and so diffuses into cytoplasm triggers the release of another messenger Ca$$^{2+}$$ ions from intracellular endoplasmic reticulum activating many calcium-mediated processes.
- While DG remains in the membrane where it activates an enzyme called protein kinase C, which in turn, activates many other enzymes, such as pyruvate dehydrogenase, and so brings about the physiological effects.
Amplification of signal

- A single subunit of insulin receptor activates many molecules of DG, and each protein kinase C molecule activated by DG will, in turn, activate many other enzyme molecules.
- DG and IP3 are examples of second messengers, intermediary compounds that amplify a hormonal signal and so set into action a variety of events within the affected cell.
- A variety of events within the affected cell.
- A variety of hormones use another second messenger, the cyclic form of adenosine monophosphate, (cAMP). The enzyme adenylate cyclase converts adenosine triphosphate (ATP) into cAMP.
- Because an enzyme can be used over and over again, a single molecule of active adenylate cyclase can catalyse production of about 100 molecules of cAMP.
- In muscle or liver cells, when hormones, such as, adrenaline bind receptors, the receptors change shape and bind to G protein, causing it, in turn, to bind the nucleotide guanosine triphosphate (GTP) and activate another protein adenylate cyclase. The result of this complex cascade of interactions is the production of large amounts of cAMP.

Comments
Post a Comment